Availity Tips: Coordination of Benefits, Vision, and Dental
Your feedback helps us make meaningful changes within Availity as quickly as possible. Here are some helpful reminders, thanks to questions we’re hearing from providers.
If you have new office staff who need Availity training, they can view the Premera Availity Tips and Resources video tutorial or check out our user guide.
Availity also offers Premera-specific webinars in the Availity Learning Center. Simply sign in to Availity, and go to the Availity Learning Center > Help & Training > Get Trained and enter the keyword “Premera.”
Coordination of benefits:
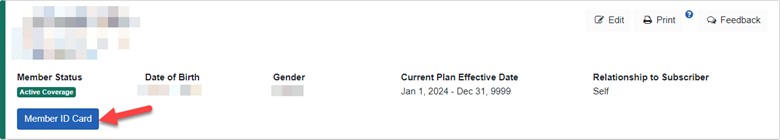
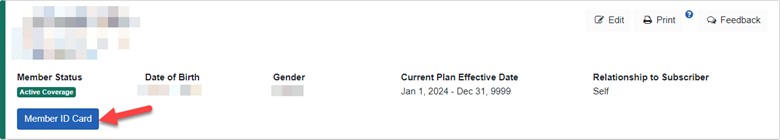
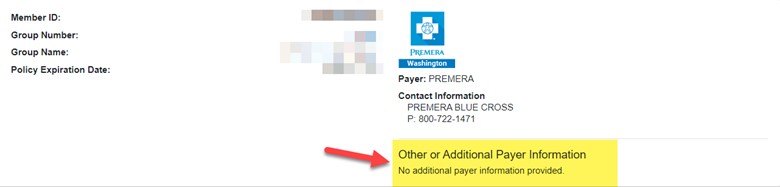
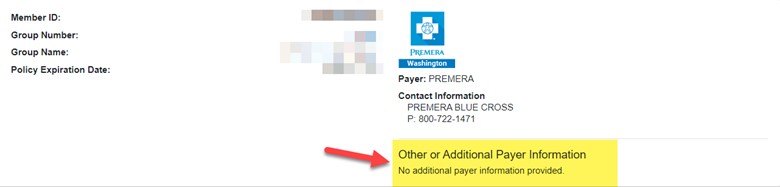
I need to check the patient’s coordination of benefits (COB). Where can I find that in Availity?
If we know a member has other insurance, we’ll provide that information under the “Other or Additional Payer Information” section located below the payer logo that displays at the top of the page:
Looking up eligibility and benefits:
Are there other options to look up eligibility and benefits? Is the only option to use the member’s ID number?
Yes, there are six different ways to verify a member’s eligibility and benefits. Under Member Search Options, you can choose from the following:


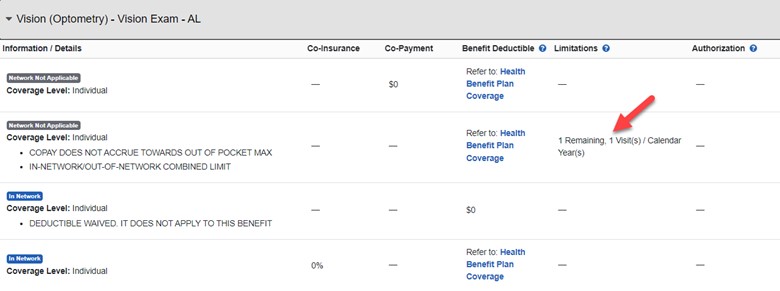
Visit limits for routine vision:
Where do I find the visit limits for routine vision services?
If there’s a visit limitation, the limitation will display under the “Limitations” section of the benefit display:
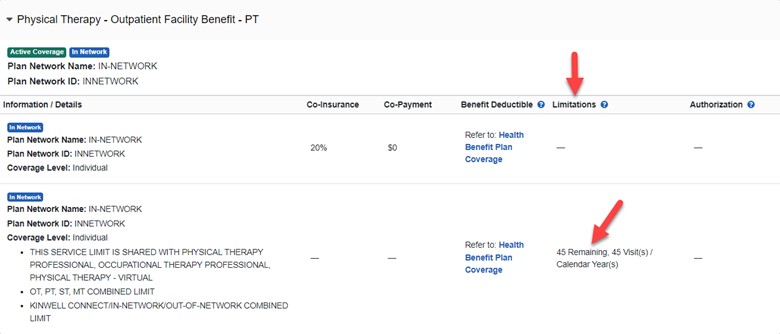
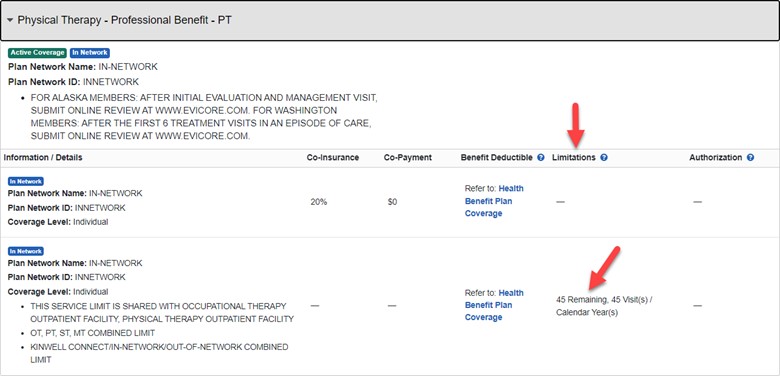
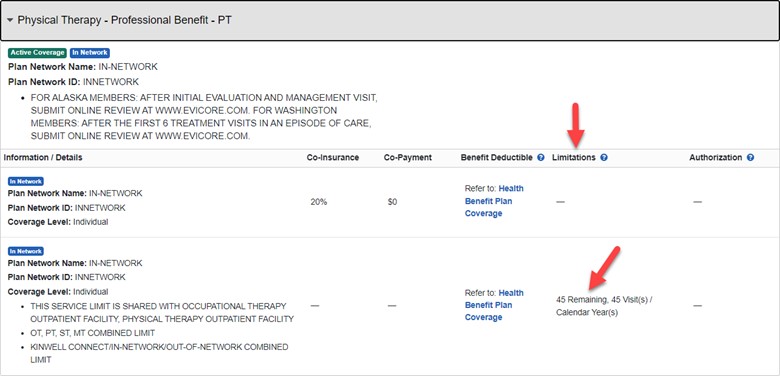
Visit limits for physical therapy:
Where do I find the visit limits for physical therapy?
If it’s not listed, there is no visit limit. If there is a limited number of visits available, you’ll see it under the heading Limitations. Here are two examples:
Dental contact information:
Where is the correct contact information for Premera Dental?
Check the back of member’s ID card. A copy of the member’s ID card displays under the Eligibility and Benefits Inquiry feature. Or go to the Premera Dental Payer Space > Resources > Contact Premera: